A Comprehensive Guide to Understanding and Diagnosing the Most Misunderstood Phase of Women’s Health

If you’re asking this question, you’re probably experiencing changes that feel confusing, overwhelming, or just… different. Maybe you’re in your late 30s or early 40s, still getting your periods, but something fundamental has shifted. Your body feels foreign. Your emotions are all over the place.
The truth is, working out if you’re in perimenopause—especially early perimenopause—is far more complex than most doctors make it sound. Getting this right matters enormously, because the wrong approach can actually make everything worse.
Why This Matters More Than Anyone’s Telling You
Here’s what I want you to understand: perimenopause is not “mini-menopause.” It’s not your body gently winding down towards the end of your fertile years. It’s a completely distinct, dynamic hormonal phase with its own rules, its own challenges, and its own treatment needs [1,16].
When doctors misunderstand this—or worse, when they treat you as if you’re already in menopause—it can lead to treatments that not only don’t help, but can make your symptoms dramatically worse.
I’ve seen women given high-dose estrogen therapy when their estrogen levels are already sky-high and erratic. The result? Worsening flooding, clotting, unbearable breast tenderness, migraines that come out of nowhere, mood swings that feel uncontrollable. Some women end up needing surgery for problems that could have been prevented with the right understanding from the start [1,5].
The stakes are higher than most people realise, and yet this phase of your life is still largely misunderstood—even by many healthcare providers.
The Hormonal Truth That Changes Everything
Let me share something that might surprise you: perimenopause is actually characterised by higher, more erratic estrogen levels, not the low estrogen state everyone talks about with menopause [1,3,4].
I know this sounds backwards from everything you’ve probably heard, but the research is crystal clear. During perimenopause, your estrogen levels can be 26% higher than they were during your regular reproductive years, swinging wildly up and down in ways that make no sense [3]. At the same time, your progesterone production is declining, creating this state we call “estrogen dominance.”
This explains so much of what you might be experiencing: the flooding periods, the tender breasts, the mood swings, the sleepless nights, the weight that seems to appear overnight, and that overwhelming feeling that your body has been taken over by someone else’s hormones [1,2].
Many women tell me they feel “pregnant” during this time—and that makes perfect sense, because high estrogen symptoms (breast tenderness, bloating, emotional sensitivity) are exactly what you experience in early pregnancy [1,4].
HIGH ESTROGEN AND LOW PROGESTERONE IN PERIMENOPAUSE
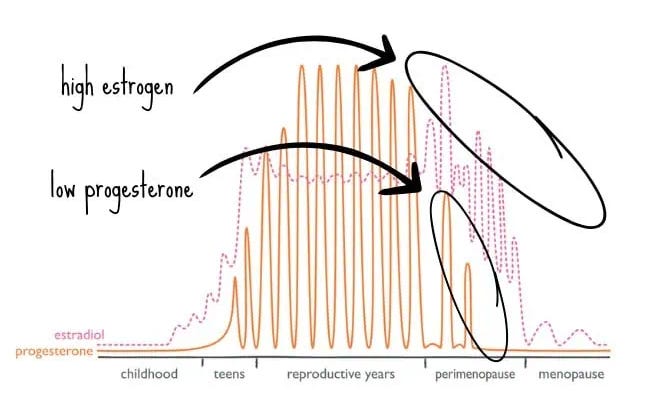
Figure 1. High estrogen and low progesterone across the female lifespan, highlighting perimenopause. Adapted from: Briden L. What estrogen does in perimenopause (and how progesterone can help). [Internet]. 2021 [cited 2025 May 26]. Available from: https://www.larabriden.com/what-estrogen-does-perimenopause-how-progesterone-can-help
ELEVATED ESTROGEN IN PERIMENOPAUSE
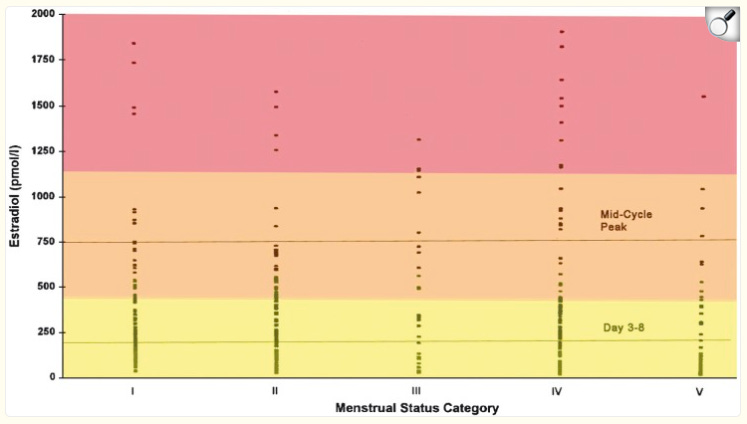
Figure 2. Cross-sectional mid-follicular phase estradiol levels by menstrual cycle characteristics in menstruating women ages 45–55, with reference lines for premenopausal mean and peak E2 levels. Reproduced from: Prior JC. Progesterone for symptomatic perimenopause treatment — progesterone politics, physiology and potential for perimenopause. Facts Views Vis Obgyn. 2011;3(2):109-120.
Early Perimenopause:
The Diagnosis Most Doctors Miss
Early perimenopause often starts in your late 30s or early 40s—sometimes even earlier. Yet it’s constantly misdiagnosed as depression, anxiety, or just “stress.” I see this in my clinic all the time [14,15]. This phase can last anywhere from 2-5 years before you move into the more obvious later stages [1,6].
Here’s the key: you can be diagnosed with early perimenopause even if you’re still having regular periods. Professor Jerilynn Prior, one of the world’s leading researchers in this area, has developed clear criteria [1]:
If you’re experiencing ANY 3 of these 9 changes, you could be in early perimenopause:
- New onset heavy and/or longer flow – Flooding, clots, changing protection more often, periods lasting more than 5-7 days
- Shorter menstrual cycles (≤ 25 days) – Your periods coming more frequently than they used to
- New sore, swollen or lumpy breasts – Cyclical breast tenderness that wasn’t there before
- New mid-sleep wakening – Waking up in the middle of the night and struggling to get back to sleep
- Increased menstrual cramps – Period pain that’s new or significantly worse
- Onset of night sweats, especially before your period – Episodes of sweating during sleep
- New or markedly increased migraine headaches – First-time migraines or existing ones getting much worse
- New or increased premenstrual mood swings – Emotional reactivity that feels out of proportion
- Weight gain without changes in diet or exercise – Especially around your middle
This framework recognises that perimenopause is defined by what’s happening in your body, not by your age [1].
Understanding the Full Journey:
The Stages Explained
Perimenopause isn’t one phase—it’s a journey through several distinct stages, each with its own hormonal patterns and symptoms [1,6,16]. Understanding where you are can help you make sense of what’s happening and what to expect.
PRIOR’S STAGES OF PERIMENOPAUSE DIAGRAM
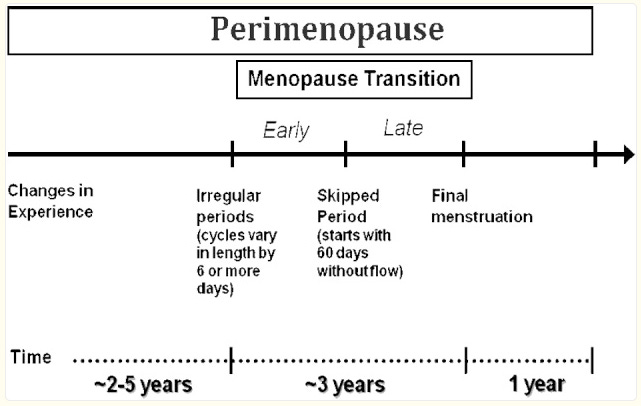
Figure 3. Stages of the perimenopausal transition. Reproduced from: Prior JC. Progesterone for symptomatic perimenopause treatment — progesterone politics, physiology and potential for perimenopause. Facts Views Vis Obgyn. 2011;3(2):109-120.
TABLE 1. PERIMENOPAUSE STAGES AND SYMPTOMS
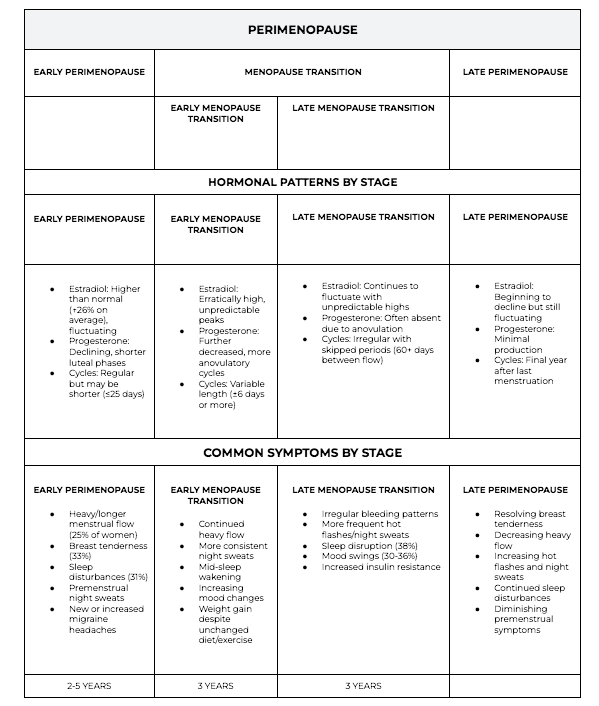
Early Perimenopause (2-5 years): Your estrogen is actually higher than normal and fluctuating wildly [3], while progesterone starts declining [4,6]. Your cycles might be regular but shorter [1]. About 25% of women experience heavy bleeding [5], 33% have breast tenderness [2], and 31% struggle with sleep [2]. This is often when premenstrual night sweats start and migraines worsen [1].
Early Menopause Transition (3 years): Estrogen continues its erratic, unpredictable peaks [3,6], progesterone drops further with more cycles where you don’t ovulate [6]. Your cycle length becomes more variable [1,6]. Heavy bleeding often continues, night sweats become more consistent, and you might find yourself waking up in the middle of the night regularly. Mood changes intensify, and weight gain can happen despite no changes in your lifestyle [1,2].
Late Menopause Transition (3 years): Estrogen is still fluctuating with unpredictable highs [6,7], but progesterone is often completely absent [6]. You start skipping periods—sometimes 60+ days between flows [17]. Bleeding patterns become irregular, hot flashes and night sweats increase, sleep disruption affects 38% of women [16], mood swings affect 30-36% of women [16], and insulin resistance often develops [1].
Late Perimenopause: Estrogen finally begins to decline but is still fluctuating [6], progesterone production is minimal [6]. This is your final year after your last period [17]. Breast tenderness starts resolving, heavy flow decreases, but hot flashes and night sweats increase. Sleep disturbances continue, though premenstrual symptoms begin to diminish [1,16].
Why Blood Tests Often Miss the Mark
One of the most frustrating experiences is being told your hormones are “normal” based on a single blood test [14,15]. I hear this from women constantly, and here’s why it happens:
Your hormones are fluctuating dramatically from day to day during perimenopause [1,3]. That “normal” result on Tuesday could be completely different on Thursday [3]. Standard lab ranges don’t account for the wild swings that are actually normal for this phase [4]. Plus, when you have your blood drawn within your cycle matters enormously [17]. I will go into helpful testing in future articles.
A proper diagnosis should include [1,17]:
- Tracking your symptoms across several cycles
- A detailed look at how your menstrual patterns have changed
- Ruling out other causes like thyroid issues
- Considering your age and individual circumstances
- Working with someone who truly understands perimenopause
The Treatment Approach That Actually Works
When you understand the real hormonal picture—high, erratic estrogen combined with declining progesterone—everything about treatment changes. This is why Professor Jerilynn Prior advocates for progesterone-only therapy during perimenopause [1,5].
Think about this: in a normal menstrual cycle, progesterone levels are 100-200 times higher than estrogen [1]. The last thing most perimenopausal women need is more estrogen.
Progesterone therapy can be transformational because it [1,8,9,10]:
- Reduces inflammation
- Stabilises estrogen’s effects
- Calms your immune system (helpful for those new allergies and sensitivities think Mcas)
- Soothes your brain, improves sleep, and reduces anxiety
- Protects your breasts, uterus, heart, bones, and helps with weight management
Red Flags: When Treatment Goes Wrong
If you’ve been treated for “menopause” and experienced any of these, you might have been given inappropriate estrogen therapy [1,5]:
- Bleeding got worse or you started clotting
- Breast tenderness increased
- Migraines worsened
- Anxiety or mood swings intensified
- New inflammatory symptoms appeared
- You developed allergic or histamine-type reactions
The Healthcare Reality: Why Getting Help Feels So Hard
If you’ve struggled to get proper help, you need to know it’s not your fault. There are real, documented problems with how the medical system handles perimenopause:
Training Gaps: In Australia, some medical students receive as little as one hour of education about menopause and perimenopause in their entire degree [11]. In the UK, 52% of GPs admit their training didn’t adequately prepare them to help women with menopausal symptoms [12].
Dismissive Attitudes: Surveys show that 39% of women seeking help for perimenopause are told they’ll “just have to live with it,” and 25% are told they’re “too young” to be perimenopausal [14].
Multiple Appointments: 36% of women need three or more GP visits before getting appropriate help [14].
System Barriers: Time constraints, lack of specialised training, and contradictory research results all contribute to inconsistent care [13,15].
These aren’t isolated problems—they’re systemic issues affecting women everywhere [11,12,13,14,15].
What This Means for You
Perimenopause is complex and dynamic, and it deserves to be understood properly, not dismissed [16]. If you recognise yourself in what I’ve described, trust your instincts. Your symptoms matter. Your experience is valid. And with the right approach, this transition can be manageable—even empowering.
The key is finding healthcare providers who understand that perimenopause isn’t menopause, who recognise the unique hormonal landscape of this phase, and who approach your care with the nuance this life stage requires [1,17,18].
Remember: you know your body better than anyone else. If something feels different, it probably is. Don’t let anyone minimise your experience or brush you off with “it’s just stress” when you know something fundamental has shifted [14,15].
Getting the right diagnosis and treatment isn’t just about surviving perimenopause—it’s about thriving through it and setting yourself up for vibrant health in the years ahead.
Recognising these early signs allows for timely, appropriate intervention that addresses the real hormonal changes happening in your body. This approach supports your natural transition while protecting your long-term health and vitality [1,16].
Your Journey Forward:
Taking Back Control
If you’ve read this far, you’re already taking the first crucial step: seeking answers instead of accepting dismissal. You’re questioning the narrative that tells you to “just live with it” or that your symptoms are “all in your head.” That’s exactly the kind of self-advocacy that leads to real change.
Here’s what I want you to take away from everything we’ve covered: perimenopause is not something that happens to you—it’s something you can understand, navigate, and even transform into a period of empowerment.
The confusion you’re feeling about whether you’re in perimenopause isn’t a reflection of your inability to understand your body. It’s a reflection of a medical system that hasn’t caught up with the science, and a culture that has failed to educate women about this crucial life phase. When you know that your estrogen is likely higher and more erratic than ever before, when you understand that your progesterone is declining, when you recognise that your symptoms make perfect biochemical sense—everything changes.
This isn’t just about getting a diagnosis. It’s about reclaiming your narrative. For too long, women have been told that feeling awful during perimenopause is just part of being female. That weight gain is inevitable. That mood swings are something you have to endure. That brain fog is normal aging. None of this is true.
Perimenopause is actually an opportunity—a biological transition that, when properly supported, can set you up for the most vibrant, healthy decades of your life. But only if you understand what’s really happening and address it appropriately.
The nine signs we discussed aren’t just diagnostic criteria—they’re your body’s way of telling you exactly what it needs. Heavy bleeding? Your estrogen dominance needs balancing. Sleep disruption? Your nervous system needs calming support. Weight gain despite no dietary changes? Your metabolism needs specific attention. These aren’t failures of your willpower or signs that you’re “falling apart”—they’re precise biological feedback.
When I work with women in my clinic, I see this transformation happen over and over again. Once they understand their hormonal reality, once they stop fighting their biology and start working with it, everything becomes possible. The flooding periods resolve. The sleep improves. The weight stabilises. The mood swings even out. The brain fog lifts.
This is what happens when you repair your gut (because so much of hormone metabolism happens there), rebalance your hormones (with the right approach for your actual hormonal state), and reclaim your metabolic health. This is the Hierarchy of Healing in action—not as a quick fix, but as a sustainable transformation that honours your body’s wisdom.
You don’t have to choose between accepting misery or taking inappropriate treatments that make things worse. There’s a third option: understanding your biology, advocating for proper care, and taking control of your health in a way that works with your body’s natural processes.
Your symptoms are valid. Your experience matters. Your instincts about your body are trustworthy. And most importantly, you have more power over how you feel than anyone has probably told you.
The road ahead might require you to educate your healthcare providers, to track your symptoms more carefully than you have before, to advocate for yourself more strongly than feels comfortable. But every woman who has walked this path before you has made it easier for the next woman to get proper care.
This isn’t just about surviving perimenopause—it’s about using this transition as a catalyst to create the healthiest, most vital version of yourself. It’s about getting off the rollercoaster of hormonal chaos and stepping into a place of understanding, control, and genuine wellbeing.
Your journey through perimenopause can become the foundation for decades of vibrant health ahead. And it starts with the simple recognition that you deserve better than suffering in silence.
Trust your body. Trust your instincts.
The next phase of your life is waiting.
And it can be extraordinary.
References
- Prior JC. Progesterone for symptomatic perimenopause treatment — progesterone politics, physiology and potential for perimenopause. Facts Views Vis Obgyn. 2011;3(2):109-120.
- Dennerstein L, Dudley EC, Hopper JL, Guthrie JR, Burger HG, Morris HA. A prospective population-based study of menopausal symptoms. Obstet Gynecol. 2000;96(3):351-8.
- Santoro N, Rosenberg J, Adel T, Carter MM. Characterization of reproductive hormonal dynamics in the perimenopause. J Clin Endocrinol Metab. 1996;81(4):1495-501.
- Prior JC. Perimenopause: The complex endocrinology of the menopausal transition. Endocr Rev. 1998;19(4):397-428.
- Moen MH, Kahn H, Bjerve KS, Halvorsen TB. Menometrorrhagia in the perimenopause is associated with increased serum estradiol. Maturitas. 2004;47(2):151-5.
- Hale GE, Hughes CL, Burger HG, Robertson DM, Fraser IS. Endocrine features of menstrual cycles in middle and late reproductive age and the menopausal transition classified according to the STRAW staging system. J Clin Endocrinol Metab. 2007;92(8):3060-7.
- Harlow SD, Mitchell ES, Crawford S, Casgrande D, Burger HG, Woods NF, et al. The ReSTAGE Collaboration: defining optimal bleeding criteria for onset of early menopausal transition. Fertil Steril. 2008;89(1):129-140.
- Schussler P, Kluge M, Yassouridis A, Dresler M, Held K, Zihl J, Steiger A. Progesterone reduces wakefulness in sleep EEG and has no effect on cognition in healthy postmenopausal women. Psychoneuroendocrinology. 2008;33(8):1124-31.
- Fournier A, Berrino F, Clavel-Chapelon F. Unequal risks for breast cancer associated with different hormone replacement therapies: results from the E3N cohort study. Breast Cancer Res Treat. 2008;107(1):103-11.
- Prior JC, Hitchcock CL. Oral micronized progesterone for vasomotor symptoms-a placebo-controlled randomized trial in healthy postmenopausal women. Menopause. 2012;19(4):406-12.
- Senate Community Affairs References Committee. Menopause inquiry recommends GP education boost. RACGP. 2025 Jan 28.
- Sivapalan S, Naz S, Rashid S, Jha P. An online survey and interview of GPs in the UK for assessing their satisfaction regarding the medical training curriculum and NICE guidelines for the management of menopause. Cureus. 2022 Sep 20;14(9):e29294.
- Kling JM, Hopkins RP, Fried LP. Barriers to the care of menopausal women. J Womens Health (Larchmt). 2018 Nov;27(11):1271-1277.
- Balance Menopause, Mumsnet, Gransnet. Women are struggling to get help from GPs for perimenopause and menopause symptoms. Balance Menopause. 2021 Oct 8.
- O’Connor M, McCarthy L, O’Mahony A, Johnston J, Hynes SM. General practitioners’ and women’s experiences of perimenopause consultations: a qualitative evidence synthesis protocol. Syst Rev. 2024;13:123.
- Santoro N, Randolph JF. Perimenopause: From Research to Practice. J Womens Health (Larchmt). 2016;25(4):332-339.
- Australasian Menopause Society. Perimenopause or Menopausal Transition. 2023 Mar 26.
- Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG). Managing menopausal symptoms. 2020.
- Briden L. What estrogen does in perimenopause (and how progesterone can help). [Internet]. 2021 [cited 2025 May 26].
READ LATEST
the





Share to: